Speech pathologists work with people with communication problems. Speech pathologists study, assess, work out the problem, give advice, give therapy, and find the right tools for you. Communication problems include problems with speaking, hearing, listening, understanding, social skills, reading, writing, and using voice. There are lots of causes for communication problems. For example brain differences from birth like autism and cerebral palsy, medical problems like cleft palate and lumps on the vocal cords, hearing loss, and brain damage from accident or illness. Communication problems can be in families and can have no known cause. A communication problem can make it hard to speak up or make decisions, learn, make friends, stay safe, and have good mental health. A communication problem can be mild to severe and can last a short time or for life. People with communication problems can be angry, embarrassed, or very sad. Get help as soon as possible as this can make a big difference.
Behaviour therapy is a form of therapy that focuses on changing behaviours in a positive and effective way. Behaviour therapy for children in Australia can help children develop their communication, social, daily living, and motor skills, overcome problematic behaviours and develop healthy habits. A behaviour therapist is a professional who specialises in behaviour therapy. They work with individuals to identify problematic behaviours and develop strategies to change those behaviours. Behaviour therapists may have training in various approaches, including Applied Behaviour Analysis (ABA) and Cognitive Behavioural Therapy (CBT).
Child counsellors can help children to understand and manage their emotions, set realistic goals, and develop coping strategies for dealing with stress. If your child is experiencing difficulties at school or home, a counsellor can provide support and guidance. Counselling can also help children who have experienced trauma or are struggling with anxiety or depression.
Child counsellors specialise in working with children and adolescents. They are trained to understand the unique challenges that young people face. They can provide support and guidance to help them deal with these challenges in a healthy way.
An allied health assistant is a healthcare professional who provides support to patients and families in a variety of settings. They may work in hospitals, clinics, or community health centres. Allied health assistants typically have an associate's degree from an accredited program.
The role of an allied health assistant is to provide support to patients and families. This may include providing transportation, scheduling appointments, and providing emotional support. They also play an important role in patient education and discharge planning.
Allied health assistants are an important part of the healthcare team. They play a vital role in supporting patients and families during their time of need.
Speech refers to how the tongue, lips, jaw, and other speech organs are involved in producing sounds and using sounds in words. Language refers to the communication of thoughts and feelings through symbols, such as sounds, gestures, or written words, which uses a set of shared rules.
Voice refers to the ability to produce sounds with the vocal cords, including the quality, pitch, and loudness of the voice. Speech fluency refers to the smoothness of speech in terms of its rate and flow. Stuttering is characterised by a high frequency or duration of stoppages in the flow of speech.
Social communication refers to the use of language within a social context, including taking turns, initiating and maintaining conversation, and modifying language for different people and situations.
Speech, language, and communication needs is the umbrella term for children who have needs in one or more of these areas and need help from their family, school, and speech pathologist.
Parent training and parent led therapy programs put you in the driver's seat to help your child grow their skills. It lets you learn how to help your child yourself. In parent training and parent led therapy programs you are not limited to the number of therapy hours your child receives. You will be able to use your learning to support your child in their everyday life. Research shows that children learn best during everyday interactions with the important adults in their lives. Evidence shows that parents learning how to assist their child’s development can be as effective and in some cases more effective than a specialist working directly one-on-one with your child. These programs are evidence-based and cost-effective.
In this approach you will set realistic and achievable goals for your child and receive strategies and resources to support your child to achieve those goals. The focus will be on increasing your child’s participation at home, at school, and in the community for long-term success.
The cost of assessment differs depending on the particular assessment or assessments completed so the costs will be provided to you before you commit to the assessment appointment. Therapy is charged at the price set by the NDIS for speech pathology therapy and is based on the length of the therapy session. Payment is due at the end of assessment and therapy sessions.
Families may wish to use funding to help pay for the cost of therapy. If you already have NDIS funding then you can use your child’s NDIS funds for assessment and therapy. Children under the age of seven may be able to get NDIS funding based on needing a range of support from multiple professionals such as speech pathologists, occupational therapists, and psychologists. Children under the age of seven do not need a diagnosis to get NDIS early childhood early intervention funding. Typically children above the age of seven do need a diagnosis to get NDIS funding or to continue to get NDIS funding. You may like to get an assessment for this purpose. NDIS funds may be managed by the NDIA (agency managed), managed by an external plan manager (plan managed), or managed by yourself (self managed).
Families may also be able to get a rebate from Medicare to cover some of the cost of assessment and therapy. You will need to get a referral from a medical professional such as a general practitioner (GP) or paediatrician to be able to get a Medicare rebate for speech pathology. A GP can start a chronic disease management plan (previously enhanced primary care plan) for a paediatrician or other specialist can write a referral with medicare items (typically Medicare item 110 or 116) to cover some of the cost of assessment. The Medicare rebate that you receive from a paediatrician or specialist is higher than the rebate from a GP (approximately $55 rebate for a referral from a GP and $77 rebate for a referral from a specialist).
Families may also be able to use their private health insurance to cover some of the cost of assessment. The amount that is covered depends on the private health insurance company so check with your private health insurer.
Only one type of funding (NDIS, Medicare, private health insurance) may be used to cover some of the cost of assessment and therapy.
Receptive language refers to the understanding of spoken and written language, e.g. following instructions, understanding the relationships between words, understanding spoken sentences, and reading comprehension.
Expressive language refers to the production of spoken and written language, e.g. vocabulary, grammar, and creating meaningful and grammatical sentences.
Children with a developmental language delay have a mild to moderate impairment in understanding (receptive) and/or using (expressive) spoken and written language compared to peers their own age. This may involve the form of language (sounds, grammar, and sentence structure), the content of language (words, word relationships), and/or the function of language in communication (social use). Children who have a developmental language disorder have a significant impairment compared to peers their own age.
Developmental Language Disorder (DLD) is a neurodevelopmental condition affecting approximately 7% of the population. The cause of DLD is generally unknown. DLD may impact behaviour, attention, academic achievement, and peer relationships.
A Developmental Language Disorder presents differently across individuals.
A diagnosis of a condition in no way changes who a child is as a person. It simply describes a cluster of observable behaviours and may help them and those around them better understand and support them as an individual.
There are many causes of communication problems. For example, brain differences from birth, like autism, Down syndrome, cerebral palsy, and hearing impairment. Sometimes communication problems can be in families or have no known cause. A communication problem can make it hard to speak up, learn, make friends, stay safe, and have good mental health. A communication impairment can be mild to severe and for a short time or for life. Early intervention can make a big difference. See Speech Pathology Australia for more information.
Language delay or disorder is different from a speech delay or disorder, which involves difficulty with speech production.
The Clinical Evaluation of Language Fundamentals, Fourth Edition (CELF-4) is a standardized language assessment tool used to identify, diagnose, and evaluate language and communication disorders in children from 5-21 years of age. It is used to identify a student’s strengths and weaknesses in receptive language skills (i.e. understanding language) and expressive language skills (i.e. language production) compared to his/her peers. It does not assess reading, writing, spelling, or mathematics, though language is the foundation for these skills and for learning in general at home and school.
Developmental language difficulties are likely to be the result of many complex interactions between genetics and the environment. It is unlikely to be related to particular parenting styles or behaviors. Research continues to explore the genetic and environmental contributions that affect language development, processing, and/or auditory perception. Additionally, language difficulties may be associated with early developmental conditions, hearing loss, or brain damage. Even though a child experiences language difficulties, we can develop his or her language abilities and support them to reduce the impact of their difficulties.
Being an English as an additional language/dialect (EAL/D) speaker does not cause a language delay or disorder. Children learning EAL/D will need varied exposure to English at home and school to acquire comparable English language skills as their English-only speaking peers. Typically, this is two to three years of formal schooling, though this is determined on an individual basis. Progress over time is a valuable indicator for determining whether the child is learning English as an additional language/dialect or is presenting with a language delay or disorder.
Some children may have difficulty in all languages they speak. In this case, the Speech-language pathologist will determine whether a language delay or disorder should be considered.
Developmental language delay or disorder occurs in approximately 10-15% of school-age children.
Oral language is the foundation upon which reading and writing develops. As such, reading and writing are both language-based skills. Typically, oral language develops first and then reading and writing is taught, building upon the vocabulary, background knowledge, and sentence structures of oral language. Therefore, a child’s early oral language abilities are strongly linked with reading, writing, and academic achievement. As a child encounters new content through reading and writing, this information also serves to enhance and extend his or her oral language skills.
Each child with a language delay or disorder has a unique profile of strengths and areas for improvement that will be taken into account when planning for your child’s learning. See your child’s report for more information. The effects of a language delay or disorder vary depending on many factors, including child, family, school, and cultural factors. Language delay or disorder is likely to be an ongoing condition with ongoing support provided at school. However, predicting a child’s future is never certain. The important task is to help your child to be the best he or she can be now.
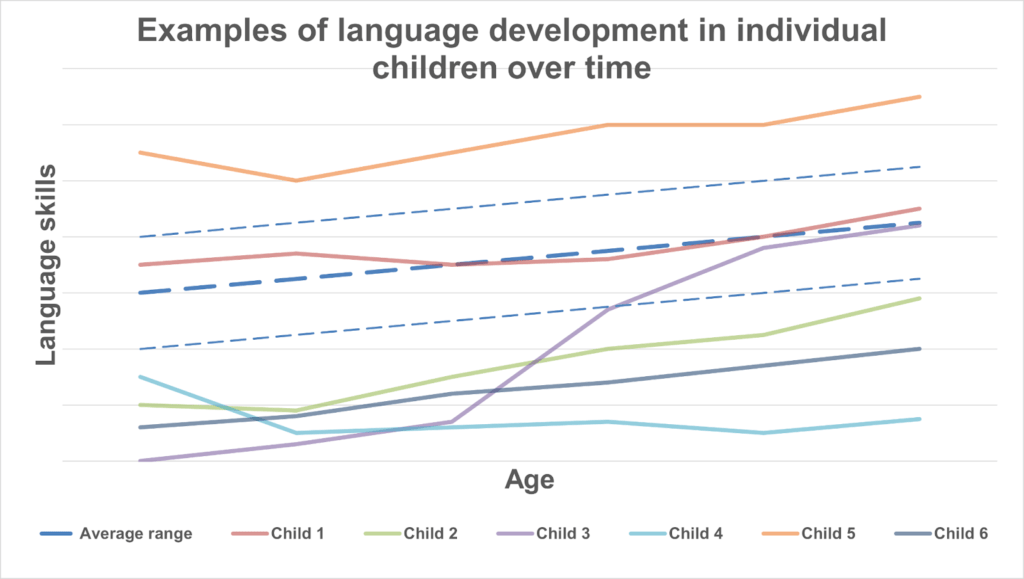
See Figure 1. This illustrates the language skills of six different children. Individual children have different language development over time. However, the average range for language skills increases over time. Thus, any child with language difficulties would need to exceed the growth rate of their peers to approach the average range, which is not an easy task. However, Child 3 does make dramatic growth, something often seen in children with English as an additional language/dialect. Across all these children, personal progress is of utmost importance. As such, the progress of Child 2 and Child 6 is very positive. Be aware that these represent particular profiles of language development and that every child is unique.
Please see your child’s report outlining the recommendations for your child’s learning at school. Many of these activities can also be completed at home, though please discuss these with your child’s teacher first. Additionally, exposure to a variety of language-rich and social environments e.g. sports, the zoo, after school club; talking about your actions e.g. when cooking, at the supermarket; and building language and social skills upon pre-existing routines e.g. story time, may prove valuable.
A formal hearing acuity assessment is needed in order to rule out the possibility of having a hearing difficulty impacting on your child’s learning, even if no hearing concerns have been raised. A hearing assessment contributes to your child’s profile of abilities and needs to be taken into account when reporting on a child’s language abilities (e.g. for the purposes of additional support).
An educational psychologist completes a cognitive assessment that investigates the thirteen thinking skills needed for learning at school. It is completed in a similar format as the language assessment. The educational psychologist will meet with you to discuss your child’s developmental history and the results of your child’s cognitive assessment. The cognitive assessment also contributes to your child’s profile of abilities and needs to be taken into account when reporting on a child’s language abilities (e.g. for the purposes of additional support).